 To better understand the health status of Arizona’s population, we partnered with the county health departments to conduct Community Health Assessments in 2014. We used the Community Health Assessments to develop a comprehensive State Health Assessment, which became basis for putting together an Arizona Health Improvement Plan (AzHIP).
To better understand the health status of Arizona’s population, we partnered with the county health departments to conduct Community Health Assessments in 2014. We used the Community Health Assessments to develop a comprehensive State Health Assessment, which became basis for putting together an Arizona Health Improvement Plan (AzHIP).
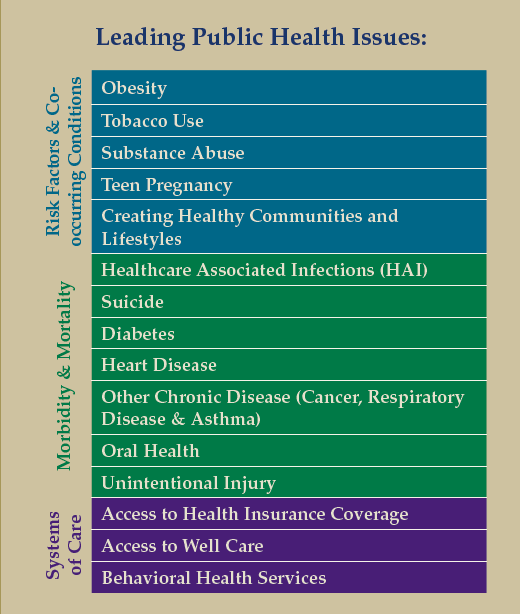
We began developing the AzHIP in late 2014 by prioritizing the 15 leading public health issues in the State Health Assessment and we’re well on our way to developing strategies to “move the needle” on the priority public health issues and to achieve improved health outcomes over the next 5 years.
The AzHIP will provide direction on how to improve the health of Arizonans in the next 5 years by aligning partnerships and resources to work collectively on shared health improvement goals and strategies. The Arizona Health Improvement Plan (AzHIP) that we finalize and begin implementing in 2015 will include: 1) Community health priorities, objectives, strategies, measures, and time framed targets; 2) Policy changes needed to accomplish objectives; 3) Individuals and organizations responsible for implementation; and 4) Measurable health outcomes or indicators.
Using our Managing Excellence executive team, we’ll be updating our Strategic Plan and Strategic Map in early 2015, aligning our top strategic priorities with the resources needed to accomplish our objectives.










This is a big problem for physicians and their reimbursement. Insurance companies must not be allowed to run their own hospitals and clinics. Their contracts are toxic to physician salaries because of their cost containment structure. Joining one network can preclude you from joining another network. In AZ where I practice as a primary care physician, BCBS has two networks Select, which is dignity health and Barrows/PCH; and Alliance which is Honor Health and Banner. The two plans force you to choose a network as a patient and offer no alternative; i.e. No PPO network. As a physician the hospitals are selective which doctors they accept as providers; i.e. If you refer patients or do procedures at a competitor network hospital more than the other network they will not allow you to be in their network. This is the case more for primary care physicians and probably not as prevalent for specialists, but the precedent has been set. Eventually, more specialists will be forced to choose what networks they work for due to the guise of cost containment.
The government needs to regulate the insurance company on this issue. The industry must be kept separate. Physicians are quietly being forced to choose selling their practice to an insurance company and likely take a pay cut so they can keep seeing patients on a particular plan or remain independent but forced off the plan and lose the patient. I am losing patients at an unprecedented rate and will eventually have to sell or contract with a specific network to be a salaried employee.
The idea of free/low cost physician visits sounds great but only if patients are permitted to see the doctor if their choosing instead of limited facility and physician networks. Obama campaigned on a promise of being able to keep your existing physician and that has not turned out to be true. More awareness needs to be brought to this alarming issue immediately both to the public and government oversight committees.
Truly,
Jeff Dare D.O., M.B.A.
Original article can be read on Medscape website titled “free physician visits with primary care doctors”