Our team is committed to connecting Arizonans with knowledge, financial assistance, and medical resources to fight disease
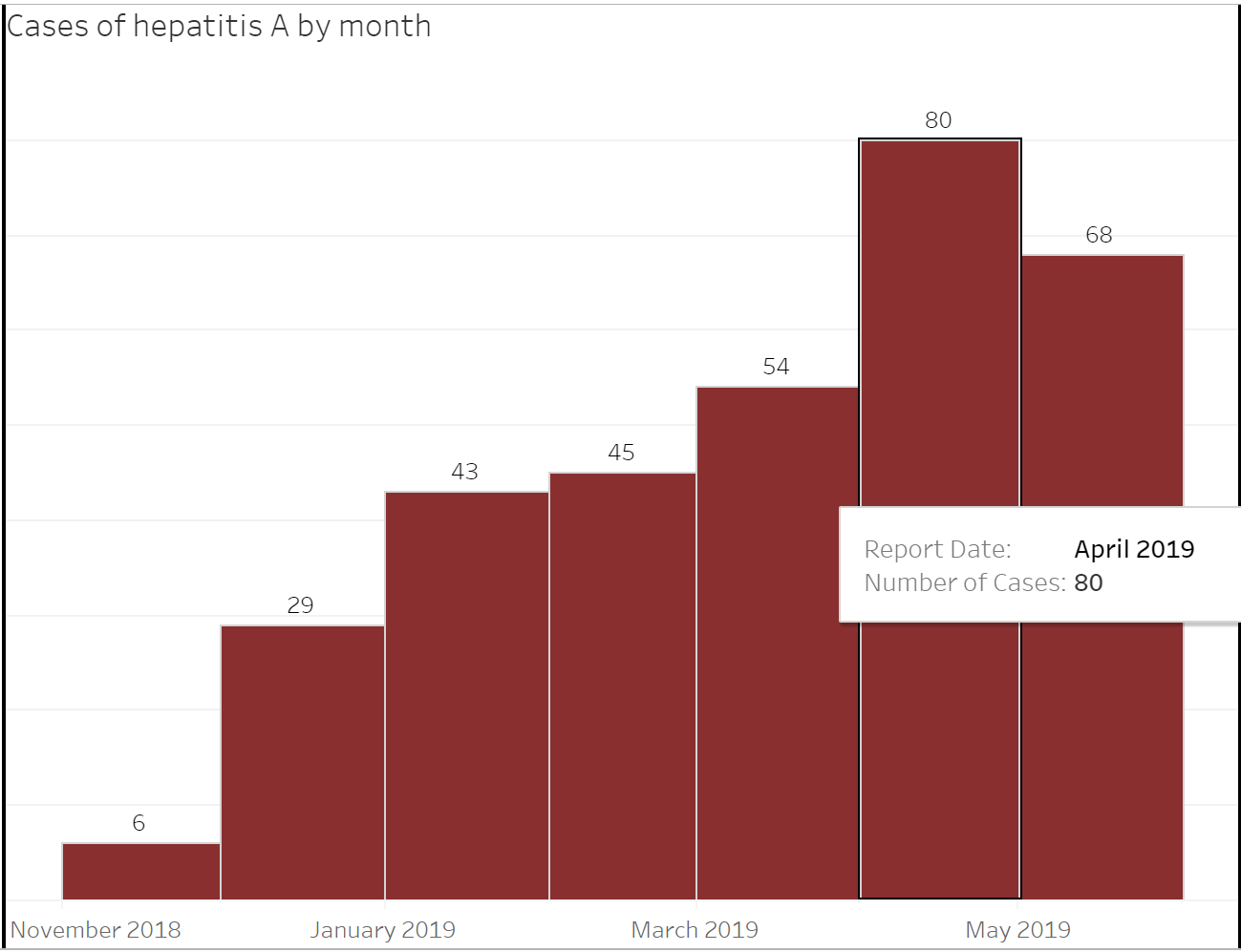
Dealing with disease can be difficult on the body, mind, and finances. In 2023, there have been 13,087 cases of reportable infectious disease so far in the state. For Arizonans combating disease, the Arizona Department of Health Services’ Office of Rapid Response Disease Investigation (ORRDI) is here to help, connecting them with assistance so they [...]